- Calls to this hotline are currently being directed to Within Health or Eating Disorder Solutions
- Representatives are standing by 24/7 to help answer your questions
- All calls are confidential and HIPAA compliant
- There is no obligation or cost to call
- Eating Disorder Hope does not receive any commissions or fees dependent upon which provider you select
- Additional treatment providers are located on our directory or samhsa.gov
Food Obsessions and the Brain: Understanding the Neuroscience of Appetite for Anorexia Nervosa
The holidays are a very difficult time for those struggling with eating disorders.
From holiday parties to gift exchanges, food is often the center attraction, towards joyous connection with family and friends. For an individual struggling with anorexia nervosa (anorexia), just the mere thought of eating can induce an adverse reaction, which is difficult to stay present and comfortable.
Kaye et al., (2003) found for those with anorexia the image of food may lead to agitation, anxiety, severe thought disturbances, and even panic. When food is nearby, negative thoughts, such as “you’re fat” or “you don’t deserve to eat that,” flood the brain of someone with anorexia.
This “noise” occurring in the brain, increases not only by the act of eating itself but also by just being around the food. These thoughts often make it difficult to engage in social interaction, and with the expectation of “eating and being merry”, the holidays for someone with anorexia can be a difficult time.
In The Presence of Food
So what happens in the brain of someone with anorexia around food? Those with anorexia tend to be harm avoidant (Kazlouski, et al., 2011). They will often avoid conflict and be overwhelmed by too much stimulus.
Becoming More Rigid
In an attempt to control their overwhelmed feelings and thoughts, a person with anorexia may become more rigid, such as counting caloric intake at every meal or weighing themselves more times throughout the day, and making fewer and fewer choices in the types of foods they eat.
Over time this repeated rigidity will show up by a decrease in the amount of activity in their life, including social isolation and more focus on eating only “safe” foods which become more and more limited.
Not Eating to Soothe
Someone with anorexia may choose not to eat, to try to soothe themselves and decrease their anxiety. As the brain starves, Serotonin decreases significantly (Kaye, 2011). This reduces the anxiety a person with anorexia may feel.
Not eating is actually a calming feature for someone who is struggling with anorexia. While most of us understand food is an important substance for nurturing life, for someone with anorexia food is mental anguish.
Moreover, when someone starts to recover and begins restoring weight, serotonin levels surge, which creates an increase in anxiety and obsessive thoughts (Kaye, 2011), making the period of weight-restoration for someone recovering an important time when they may need the most support.
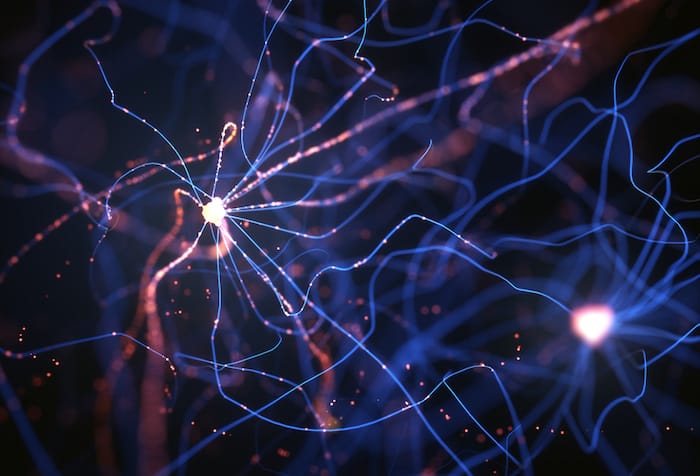
The Parts of the Brain that Relate
Researchers have identified certain parts of the brain involved with anxiety, hunger and appetite, and alexithymia (the inability to feel and express emotions) for those with anorexia.
A study by Holsen, et al. (2012) found hypo-activation (slowing down) in the hypothalamus (the body’s thermostat detecting hunger), amygdala (fear response region of the brain), and anterior insula (part of the brain responsible for interoceptive awareness including body and emotions) for both participants with active anorexia and weigh-restored participants compared to healthy-weight controls before eating.
Decreasing “Hunger” within the Brain
This suggests there is an internal mechanism within the anorexic brain that is decreasing appetite and the ability to detect hunger.
However, this hypo-activation in the anterior insula did not persist in weight-restored participants, suggesting those in recovery may regain the ability to regulate their hunger following food intake but may take longer to regain appetite signals.
The Anxious Brain
The study also suggested activation in the hypothalamus, amygdala, and anterior insula for those weight-restored were associated with hedonic (desire for favorite foods) and nonhedonic (hunger) aspects of appetite.
It is thought that dysfunction in this region of the brain for those with anorexia may reflect the anxious response to the mere idea of food. And reduced activation in the anterior insula is associated with the inability to self-awareness, such as being in a state of hunger, emotions, and other somatic sensations.
Food Does Not Stimulate the Appetite
A further study by Brooks, et al. (2012) reported those with anorexia have an increased top-down, prefrontal cortex (thinking and decision-making part of the brain) combined with reduced bottom-up somatosensory (body awareness; appetite) response around images of food.
They suggested asking those with anorexia to think about eating food does not activate appetite regions of the brain (bottom-up) and is likely to induce an appetite-aversion response (top-down).
The Role of Cognition
They examined the role of cognition (thoughts about eating) for appetite-related activation in those with anorexia and found thoughts around food for those with anorexia corresponded to reduced activation in the cerebellar vermis and increase activation in the visual cortex.
They also found those with anorexia fail to efficiently process information from appetite regions of the brain and effectively orchestrate higher-order cognitions (thoughts).
Increased Visual Cortex Activation
For a person with anorexia activation of top-down brain regions may be associated with attempts to control thoughts or disrupt somatic responses to hunger or interoceptive awareness around appetite.
Furthermore, increased visual cortex activation may be related to aversive thoughts about consuming food, when food is in sight, which overwhelms their system.
That is, thinking about eating while viewing images of food (or being around food during the holidays) conflicts with strong anxiety-provoking desires to be thin. In the study by Brooks et al, engaging participants while presenting food images by asking them to think about eating the food-induced significantly higher levels of anxiety (shown by activation in the amygdala).
Understanding the Frustrations that Food Brings
If you are recovering from anorexia, the holidays are a time to be gentle with yourself. An important first step in awareness is understanding the frustrations that food alone may bring. You can challenge the negative thoughts you may be experiencing, by finding new traditions to enjoy during the holidays.
Remaining engaged with family and friends can be difficult at times, and you may need plenty of rest and breaks. Remember to be authentic to the emotions you are experiencing. Reaching out for support during this time, even when it’s the last thing you want to do, is important for your recovery.
Families can support loved ones by knowing the difficulty they may be experiencing and making themselves more available.
Contributor: Christina Weiss, MPHC, MFTI, Primary Therapist – Shoreline Center for Eating Disorder Treatment
References:
- Brooks, S.J.,O’Daly, O., Uher, O., Friederich, H.C., Giampietro, V., Brammer, M., Williams, S. C.R.,
Schio, H.B., Treasure, J., Campbell, I.C. (2012) Thinking about eating food activates visual cortex
with reduced bilateral cerebellar activation in females with anorexia nervosa: An fMRI Study,
PLoS ONE 7(3), 2 – 11. - Holsen, L.M. PhD; Lawson, E.A., Blum, J., Ko, E. Makris, N., Fazeli, P.K., Klibanski, A. & Goldstein, J.M.
(2012). Food motivation circuitry hypoactivation related to hedonic and nonhedonic aspects of
hunger and satiety in women with active anorexia nervosa and weight-restored women with
anorexia nervosa. Journal of Psychiatry Neuroscience, 37(5), 322-32. - Kaye, W.H., Barbarich, N.C., Putnam, K., Gendall, K.A., Fernstrom, J., Fernstrom, M., Kishore, A. (2003).
Anxiolytic effects of acute tryptophan depletion in anorexia nervosa. International Journal of Eating Disorders, 33, 257–267. - Kazlouski, D., Rollin, M.D., Tregellas, J., Shott, M.E., Jappe, L.M., Hagman, J.O., Frank, G.K. (2011).
Altered fimbria-fornix white matter integrity in anorexia nervosa predicts harm avoidance.
Psychiatry Research: Neuroimaging 192, 109-116.
The opinions and views of our guest contributors are shared to provide a broad perspective of eating disorders. These are not necessarily the views of Eating Disorder Hope, but an effort to offer discussion of various issues by different concerned individuals.
Last Updated & Reviewed By: Jacquelyn Ekern, MS, LPC on December 31st, 2014
Published on EatingDisorderHope.com
Articles on Anorexia
- Anorexia and the Brain: What Do We Know?
- Instant (Chemical) Messenger: Anorexia and the Chemical Communication of the Brain
- Understanding Anorexia Treatment: What to Expect During the First Week in Residential Treatment
- Anorexia and Emotions: A Treatment Approach From the Inside Out
- Anorexia Recovery and Overcoming Physical Side Effects of an Eating Disorder
- Common Signs & Symptoms of Anorexia
- Does Anorexia Impair One’s Ability to Relate Socially?
- Anorexia and Infertility: Causation or Correlation
- A Whopping 95% of all Diets Fail: Is it Anorexia in the Making?
- Anorexia & BMI: Is Weight the Sole Determiner of Anorexia?