- Calls to this hotline are currently being directed to Within Health or Eating Disorder Solutions
- Representatives are standing by 24/7 to help answer your questions
- All calls are confidential and HIPAA compliant
- There is no obligation or cost to call
- Eating Disorder Hope does not receive any commissions or fees dependent upon which provider you select
- Additional treatment providers are located on our directory or samhsa.gov
Eating Disorders in Teens
Eating disorders are harrowing disorders that impact an individual’s medical and mental well-being, often consuming their everyday lives, relationships, and functioning. These disorders impact teens at alarmingly high rates, with the latest research from the National Institute of Mental Health indicating that 2.7% of teens will struggle with a diagnosable eating disorder [1]. If you find this alarming, consider that the number of those that do not seek help or meet full criteria for diagnosis means the prevalence is actually much higher. In fact, eating disorders are the third most diagnosed chronic illness in teens [2].
Understanding and recognizing eating disorder risk and symptoms in teens can be critically important in early intervention, which increases an individual’s likelihood of achieving full recovery.
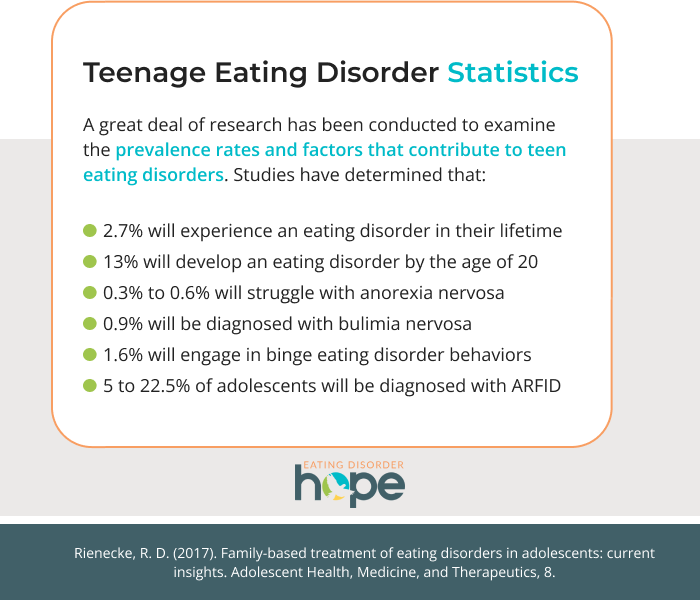
Teenage Eating Disorder Statistics
The average onset of eating disorder beliefs and behaviors occurs in adolescence, therefore, a great deal of research has been conducted to examine the prevalence rates and factors that contribute to this pattern. Studies have determined that:
- 2.7% of teens will experience an eating disorder in their lifetime [1].
- 13% of adolescents will develop an eating disorder by the age of 20 [2].
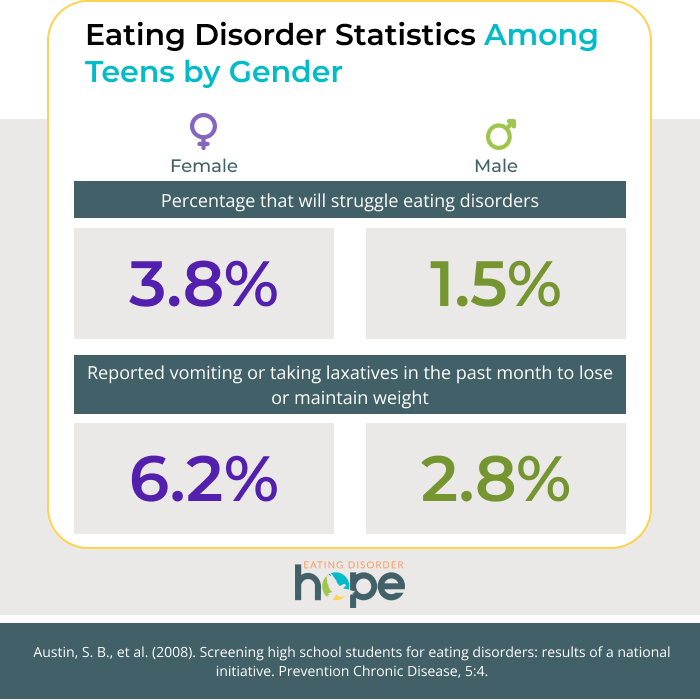
- 3.8% of female, and 1.5% of male, adolescents will struggle with an eating disorder [1].
- Prevalence rates of eating disorder diagnoses increase with age [1].
- .3% to .6% of adolescents will struggle with anorexia nervosa [2].
- .9% of teens will be diagnosed with bulimia nervosa [2].
- 1.6% of teens will engage in binge eating disorder symptoms and behaviors [2].
- 5 to 22.5% of adolescents will be diagnosed with Avoidant Restrictive Food Intake Disorder (ARFID) [2].
- In a study conducted by the Youth Risk Behavior Surveillance System (YRBSS), “6.2% of girls and 2.8% of boys reported vomiting or taking laxatives in the past month to lose or maintain weight [3].”
Types of Eating Disorders in Teenagers
The statistics above make it clear that teens are susceptible to any variation of disordered eating behaviors. Recognizing the warning signs of eating disorder behaviors may allow you to more effectively support the teens in your life.
Early Signs of Anorexia in Teenagers
Anorexia Nervosa is a dangerous and concerning disorder that involves an individual severely restricting food intake with the intent of losing weight.
With the highest mortality rate of any mental illness, recognizing signs and intervening early-on in the disorder is key to successful and long-term recovery. Teens vulnerable to anorexia nervosa may display the following:
- Reporting an intense fear of gaining weight or becoming fat.
- Preoccupation with body weight, size, and/or shape.
- Calorie counting.
- Declining/skipping meals.
- Refusing to eat in front of or with others.
- Distorted body image.
- Unusual eating habits.
- Food rules/avoidance of certain foods.
- Preoccupation with food content/ingredients.
- Insomnia.
- Irritability.
- Dry skin/hair.
- Extreme weight loss.
Binge Eating Disorder in Teens
Binge Eating Disorder (BED) involves an individual eating an atypically large amount of food in a short period of time. Individuals often feel out of control when binging and report experiencing shame and guilt afterward. BED differs from bulimia nervosa in that the individual does not engage in any compensatory behaviors to “make up” for the binge. 1.6% of adolescents will engage in these behaviors. Teens struggling with BED may exhibit the following warning signs:
- Eating in secret.
- Hiding food.
- Eating beyond fullness or until uncomfortably full.
- Eating at a fast pace.
- Reported feeling of low self-worth.
- Increased depressive symptoms.
- Weight fluctuations.
Bulimic Symptoms in Teenagers
Bulimia nervosa is characterized by episodes of binge eating followed by compensatory behaviors such as purging, fasting, or excessive exercise. Bulimia nervosa is common in adolescents and can be incredibly dangerous due to the impact such behaviors have on the physical body. Signs that might indicate a teen is struggling with bulimia nervosa include:
- Distorted body image.
- Preoccupation with body weight, shape, and/or size.
- Eating in secret.
- Hiding food.
- Eating beyond fullness or until uncomfortably full.
- Unusual eating habits/food rules.
- Expressing shame or guilt around eating.
- Frequently going to the bathroom before, during, or after meals.
- Purchasing/possessing diuretics/laxatives.
- Engage in excessive or compulsive exercise, particularly if exercise continues through fatigue or injury or in inclement weather.
- Drinking excessive amounts of water.
- Scarring on the knuckles from purging.
How Eating Disorders Impact Teens
Teens are in a crucial developmental transition during which their bodies and minds require proper nourishment to optimally function and support their growth. Eating disorder behaviors lead to malnourishment which can cause severe health consequences such as:
- Damage to vital organs.
- Loss of menstrual cycle and/or infertility in women.
- Cardiovascular complications & increased risk of heart failure.
- Severe impact on daily life functioning.
- Difficulty focusing.
- Bone and muscle loss.
- Dry skin/brittle hair.
- Increased symptoms of other mental illnesses such as Major Depressive Disorder, Generalized Anxiety Disorder, PTSD, substance use, etc.
- Gum disease and/or tooth decay/loss.
- Low bone density.
- Ulcers.
- Damage to esophageal sphincter and esophagus.
What Causes Eating Disorders in Teens?
Many environmental, psychological, biological, and social aspects can contribute to disordered relationships with food and the body. One of these factors relates to the transitional period of puberty, which involves rapid changes in the physical body that are often bewildering and overwhelming to teens. This period also causes more extreme mood swings, leaving teens feeling out of control and unlike themselves. Many may seek eating disorder behaviors as a method of coping or regaining control.
Related Reading
Social messages via movies, television, advertisements, and social media also play a part in the development of distorted beliefs around the body, weight, worth, food, and exercise. One study learned that “the greatest decline in body satisfaction occurred in girls under the age of 19 following exposure to overtly thin media images [4].” Studies also “indicate that current diet, exercise, and beauty trends displayed in reality television shows and social media outlets can contribute to unhealthy adolescent body perceptions [4].” With all of this, it is no wonder that “as many as 70% of adolescent girls would like to have a smaller body size [5].”

Adolescence also involves increased pressures to fit in socially, as the process of finding one’s identity separate from their family of origin begins, teens feel a stronger desire to belong in their peer groups. Combining the tumultuous bodily changes of adolescence with unrealistic societal expectations of the body and appearance and you have a dangerous combination of factors that lead to ineffective coping skills and concerning behaviors to change oneself to fit in.
Finally, teens experience a great deal of scholastic pressure that can contribute to emotional dysregulation, leading to the development of disordered eating and exercising behaviors as maladaptive coping skills. Teens with perfectionist and rigid tendencies, low self-worth, and/or comorbid mental health diagnoses are more likely to develop an eating disorder as well.
Teen Eating Disorder Treatment
With approximately 1 in 4 girls and 1 in 10 boys reporting at least “1 disordered eating or weight control symptom serious enough to warrant further evaluation by a health professional,” early intervention and effective treatment is key to interfering with contributing factors and reducing the risk of full diagnosis [3].
Evidence largely supports treating eating disorders in both teens and adults with Cognitive Behavioral Therapy interventions. For teens, specifically, research overwhelmingly supports the involvement of the family in treatment and recovery. A method is known as The Maudsley Method, or “Family-Based Treatment,” is encouraged to involve the family dynamic as part of the treatment process. This treatment is considered the first-line treatment for many practitioners treating adolescents with eating disorders and has proven effective with many variations of eating disorder behaviors.
Treatment can be difficult for teens as the severity of their disorder may require them to admit to an inpatient hospital for medical stabilization or a residential treatment center. Being away from home and taking a step back from their daily life will undoubtedly be challenging, however, receiving the necessary level of care as soon as possible greatly increases the likelihood of long-term recovery.
Resources
[1] Unknown (2017). Eating disorders. National Institute of Mental Health. Retrieved from https://www.nimh.nih.gov/health/statistics/eating-disorders#part_155062.[2] Rienecke, R. D. (2017). Family-based treatment of eating disorders in adolescents: current insights. Adolescent Health, Medicine, and Therapeutics, 8.
[3] Austin, S. B., et al. (2008). Screening high school students for eating disorders: results of a national initiative. Prevention Chronic Disease, 5:4.
[4] Voelker, D. K., Reel, J.J., Greenleaf, C. (2015). Weight status and body image perceptions in adolescents: current perspectives. Adolescent Health, Medicine, and Therapeutics, 6.
[5] Izydorczyk, B., Sitnik-Warchulska, K. (2018). Sociocultural appearance standards and risk factors for eating disorders in adolescents and women of various ages. Frontiers in Psychology.
Author: Margot Rittenhouse, MS, NCC
Page Last Reviewed and Updated By: Jacquelyn Ekern, MS, LPC on August 4, 2021
