- Calls to this hotline are currently being directed to Within Health or Eating Disorder Solutions
- Representatives are standing by 24/7 to help answer your questions
- All calls are confidential and HIPAA compliant
- There is no obligation or cost to call
- Eating Disorder Hope does not receive any commissions or fees dependent upon which provider you select
- Additional treatment providers are located on our directory or samhsa.gov
Anorexia’s Impact on Thinking
We have all experienced the physical and mental changes that come with hunger. Feelings of irritability, brain fog, and fatigue can make daily tasks and encounters more taxing and difficult. For those struggling with anorexia nervosa, these symptoms are more constant and more severe. Just as a starving person does not function optimally, neither does a starving brain.
Starved Body, Starved Mind
How we process and respond to information is heavily impacted by our nourishment. More specifically, research has found evidence associating anorexia nervosa “with adverse effects on cognitive functioning in the domains of attention, processing speed, visual and verbal memory, and visuospatial construction (1).”
If you’re thinking that these all sound like incredibly important areas of functioning, you are correct. An individual’s ability to process and retain information is crucial to daily life, whether in school, at a job, or simply adapting to one’s surroundings while walking, driving, or going to the grocery store.
Imagine moments when you have felt overwhelmed, hungry, or fatigued and attempt to recall how it felt in your mind. Perhaps you found it difficult to recall information that is normally first-hand knowledge to you. Maybe expressing your emotions or thoughts to another felt particularly challenging. It’s possible that being productive or effective in your goals just didn’t feel possible with where you were mentally.
These are all side-effects of a brain that is malnourished and can impact one’s job, school, relationships, and daily activities.
Not only that, these symptoms of a starved brain impact how an individual experiences treatment, as they are not cognitively capable of processing information and forming logical connections between their thoughts, beliefs, and behaviors.
One study aptly points this out in stating that “severely ill patients may not be able to fully participate in current standard of care psychotherapies because they are largely cognitive-based (1).”
Energy level is also impacted, making it hard for those struggling to muster the energy needed to engage in the important, challenging, and mentally tiring tasks needed to move toward recovery.
Long-Term Impact of Anorexia on the Brain
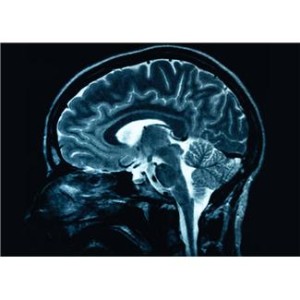
The grey matter is an important part of the brain, containing “most of the brain’s neuronal cell bodies” and including “regions of the brain involved in muscle control and sensory perceptions such as seeing and hearing, memory, emotions, speech, decision making, and self-control (3).”
As one study summarized, “grey matter plays the most significant part in allowing humans to function normally daily (4).” While weight restoration can help some of the cognitive consequences of anorexia nervosa, studies indicate that this is not always the case, finding that “impairments in the cognitive domain of memory performance persist after weight restoration (1).”
Even so, research is providing us with more insight daily, and a 2020 study found hopeful results that indicated “no clinically meaningful decrement in cognitive functioning” after medical stabilization (1). Whether these negative impacts are long-standing or not, it is clear that a malnourished body results in a malnourished mind which will struggle to function optimally.
This acts as an important reminder that food is so much more than our culture treats it. It is what fuels our bodies and gives us the capability to engage in a full and meaningful life.
References
[1] Rylander, M. et al. (2020). Evaluation of cognitive function in patients with severe anorexia nervosa before and after medical stabilization. Journal of Eating Disorders, 8:35. [2.] Fonville, L. et al. (2014). Alterations in brain structure in adults with anorexia nervosa and the impact of illness duration. Psychological Medicine, 44:9. [3.] Unknown (2020). Grey matter. Retrieved from https://en.m.wikipedia.org/wiki/Grey_matter#Function. [4.] Mercadante, A.A., Tadi, P. (2020). Neuroanatomy, grey matter. StatPearls.About the Author:

As a freelance writer for Eating Disorder Hope and Addiction Hope and a mentor with MentorConnect, Margot is a passionate eating disorder advocate, committed to de-stigmatizing these illnesses while showing support for those struggling through mentoring, writing, and volunteering. Margot has a Master’s of Science in Clinical Mental Health Counseling from Johns Hopkins University.
The opinions and views of our guest contributors are shared to provide a broad perspective on eating disorders. These are not necessarily the views of Eating Disorder Hope, but an effort to offer a discussion of various issues by different concerned individuals.
We at Eating Disorder Hope understand that eating disorders result from a combination of environmental and genetic factors. If you or a loved one are suffering from an eating disorder, please know that there is hope for you, and seek immediate professional help.
Published September 25, 2020, on EatingDisorderHope.com
Reviewed & Approved on September 25, 2020, by Jacquelyn Ekern MS, LPC
